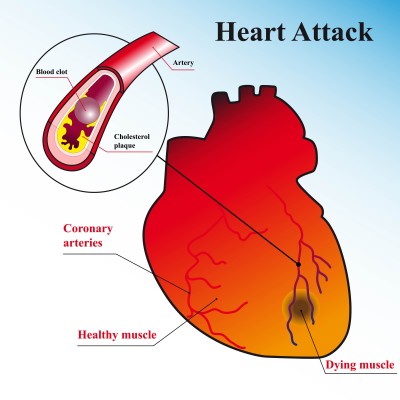
Coronary heart disease (CHD) is the leading cause of death for both men and women in the United States. CHD is caused by a narrowing of the coronary arteries that supply blood to the heart, and often results in a heart attack.
Each year, about 1.1 million Americans suffer a heart attack. About 460,000 of those heart attacks are fatal. About half of those deaths occur within 1 hour of the start of symptoms and before the person reaches the hospital.
Fortunately, everyone can take steps to protect their heart and their life or that of someone else. The key is seeking medical care as soon as possible.
This Web page tells you about heart attack and the steps you can take to increase your chances of survival. You’ll learn why a fast response to the signs of a heart attack is crucial to save lives and limit heart damage.
Heart Attack Warning Signs
Some heart attacks are sudden and intense the “movie heart attack,” where no one doubts what’s happening. But most heart attacks start slowly, with mild pain or discomfort. Often people affected aren’t sure what’s wrong and wait too long before getting help. Here are signs that can mean a heart attack is happening:
- Chest discomfort – Most heart attacks involve discomfort in the center of the chest that lasts more than a few minutes, or that goes away and comes back. It can feel like uncomfortable pressure, squeezing, fullness or pain.
- Discomfort in other areas of the upper body – Symptoms can include pain or discomfort in one or both arms, the back, neck, jaw or stomach.
- Shortness of breath with or without chest discomfort.
- Other signs may include breaking out in a cold sweat, nausea or lightheadedness
As with men, women’s most common heart attack symptom is chest pain or discomfort. But women are somewhat more likely than men to experience some of the other common symptoms, particularly shortness of breath, nausea/vomiting, and back or jaw pain.
Learn the signs, but remember this: Even if you’re not sure it’s a heart attack, have it checked out (tell a doctor about your symptoms). Minutes matter! Fast action can save lives” maybe your own. Don’t wait more than five minutes to call 9-1-1 or your emergency response number.
Calling 9-1-1 is almost always the fastest way to get lifesaving treatment. Emergency medical services (EMS) staff can begin treatment when they arrive up to an hour sooner than if someone gets to the hospital by car. EMS staff are also trained to revive someone whose heart has stopped. Patients with chest pain who arrive by ambulance usually receive faster treatment at the hospital, too. It is best to call EMS for rapid transport to the emergency room.
Stroke Warning Signs
If you or someone with you has one or more of these signs, don’t delay!
- Sudden numbness or weakness of the face, arm or leg, especially on one side of the body
- Sudden confusion, trouble speaking or understanding
- Sudden trouble seeing in one or both eyes
- Sudden trouble walking, dizziness, loss of balance or coordination
- Sudden, severe headache with no known cause
Immediately call 9-1-1 or your emergency response number so an ambulance (ideally with advanced life support) can be sent for you. Also, check the time so you’ll know when the first symptoms appeared. It’s very important to take immediate action. If given within three hours of the start of symptoms, a clot-busting drug called tissue plasminogen activator (tPA) can reduce long-term disability for the most common type of stroke. tPA is the only FDA-approved medication for the treatment of stroke within three hours of stroke symptom onset.
A TIA, or transient ischemic attack, is a “warning stroke” or “mini-stroke” that produces stroke-like symptoms but no lasting damage. Recognizing and treating TIAs can reduce your risk of a major stroke. The usual TIA symptoms are the same as those of stroke, only temporary. The short duration of these symptoms and lack of permanent brain injury is the main difference between TIA and stroke.
Cardiac arrest strikes immediately and without warning. Here are the signs:
- Sudden loss of responsiveness (no response to tapping on shoulders).
- No normal breathing (the victim does not take a normal breath when you tilt the head up and check for at least five seconds).
If these signs of cardiac arrest are present, tell someone to call 9-1-1 or your emergency response number and get an AED (if one is available) and you begin CPR immediately.
If you are alone with an adult who has these signs of cardiac arrest, call 9-1-1 and get an AED (if one is available) before you begin CPR. Use an AED as soon as it arrives.
Dial 9-1-1 Fast
Heart attack and stroke are life-and-death emergencies every second counts. If you see or have any of the listed symptoms, immediately call 9-1-1 or your emergency response number. Not all these signs occur in every heart attack or stroke. Sometimes they go away and return. If some occur, get help fast! Today heart attack and stroke victims can benefit from new medications and treatments unavailable to patients in years past. For example, clot-busting drugs can stop some heart attacks and strokes in progress, reducing disability and saving lives. But to be effective, these drugs must be given relatively quickly after heart attack or stroke symptoms first appear. So again, don’t delay get help right away!
Statistics
Coronary heart disease is the No. 1 cause of death in the United States. Stroke is the No. 3 cause of death in the United States and a leading cause of serious disability. That’s why it’s so important to reduce your risk factors, know the warning signs, and know how to respond quickly and properly if warning signs occur.
Act in Time
The American Heart Association and the National Heart, Lung, and Blood Institute have launched a new “Act in Time” campaign to increase people’s awareness of heart attack and the importance of calling 9-1-1 immediately at the onset of heart attack symptoms. Find the links here.
A Coronary Angiogram is a test that uses X-rays to help your doctor find narrowing or blockage in one or more of your coronary arteries. To perform an angiogram, a guide wire is inserted into the femoral artery of the leg and threaded up into the aorta. A catheter is then inserted along the guide wire. Once in place, a dye that is visible by X-rays (contrast dye) is injected into the bloodstream. Areas of narrowing can then be seen on a video screen and recorded. This procedure is done as part of the cardiac catheterization procedure.
Coronary Angioplasty (also called percutaneous coronary intervention or PCI) is a procedure that opens up narrowed or blocked segments of the arteries that supply blood to your heart muscle and the coronary arteries. A catheter with an empty balloon on its tip is guided into the narrowed part of the artery. The balloon is inflated to open the narrowed artery and flatten the plaque against the artery wall.
Coronary Artery Disease: While the majority of patients with typical coronary artery disease (fig. on left, coronary blockage denoted by red arrow) can be treated by percutaneous interventions or bypass surgery, there are an increasing number of patients with diffuse coronary artery disease (fig. on right) that are not candidates for such interventions.
By,
Dr Ashokan, MBBS